MEDICATION ERRORS IN NURSING: COMMON TYPES, CAUSES, AND PREVENTION
Healthcare workers face more challenges today than ever before. Doctors are seeing more patients every hour of every day, and all healthcare staff, including doctors, nurses, and administrators, must adapt to the demands of new technology in healthcare, such as electronic health records (EHR) systems and Computerized Provider (Physician) Order Entry (CPOE) systems.


Overwork and systemic issues can and do lead to medical errors-thousands, in fact, every year, according to a 1999 report by the Institute of Medicine. At the time of the report, between 44,000 and 98,000 deaths occurred each year as a result of medical mistakes.1
Today the numbers are even more alarming; according to Medcom Trainex.2 Consider the following:
- As many as 400,000 Americans succumb to medical errors annually.
- Another 10,000 people suffer complications every day.
- The total cost of these errors, including lost income and productivity, disability, and the expense of additional care, is estimated at between $17 billion and $29 billion per year.
Medical errors are not only monetarily costly, but costly in terms of loss of trust in the healthcare system by patients, reduced patient satisfaction, and degraded morale among healthcare professionals, who often feel helpless to change the situation.
It’s important to note that one of the main conclusions of the Institute’s report is that the majority of medical errors occur not as a result of incompetence or recklessness on the part of nurses and other healthcare workers, but rather as a result of faulty systems, fragmented processes, and working conditions (e.g., nurses exhausted from working double shifts).
Deaths resulting from medical errors are tragic not only for patients and their families, but for the healthcare professionals who are responsible, as an article painfully highlighted about one nurse’s tragic mistake a few years ago.
There are many types of medical errors, and they can occur anywhere in the healthcare system-from hospitals, to nursing homes, to pharmacies. The focus of this article is on medication errors in nursing. We’ll examine different types of medication errors, how they occur, and prevention measures for reducing these errors.


FRAGMENTATION AND DECENTRALIZATION: KEY PROBLEMS IN HEALTHCARE
The fragmented nature of our healthcare system has contributed to an epidemic of medication and other medical errors today. When patients see multiple healthcare providers in different settings-whether by choice or otherwise-the result is often fragmentation of information. One doctor may not have access to the same patient information as another-one of the primary causes of medication errors.
Medication Error Statistics
Seventy percent of individuals in the U.S. take at least one medication per day, and more than half of all Americans take two.3 Every day at least one death in the U.S. happens a result of a medication error, and approximately1.3 million people annually are injured due to medication errors. 4
TYPES OF MEDICATION ERRORS
Medication errors can occur anywhere along the route, from the clinician who prescribes the medication to the healthcare professional who administers the medication.
The different types of medication errors include (but are not necessarily limited to):
- Prescribing errors , wherein the selection of a drug is incorrect based on the patient’s allergies or other indications. Additionally, the wrong dose, form, quantity, route (oral vs intravenous), concentration, or rate of admission could be used.
- Omission errors , in which there is a failure to give a medication dose before the next one is scheduled.
- Wrong time errors , wherein a medication is given outside the predetermined interval from its scheduled time.
- Improper dosing errors , wherein a greater or lesser amount of a medication is delivered than is required to manage the patient’s condition.
- Wrong dose errors , wherein the correct dosage was prescribed, but the wrong dose was administered.
- Improper administration technique errors , such as administering a medication intravenously instead of orally.
- Wrong drug preparation errors , wherein a medication is incorrectly formulated (i.e., too much or too little diluting solution added when a medication is reconstituted).
- Fragmented care errors , wherein a lack of communication exists between the prescribing physician and other healthcare professionals.
These are just some of the many possible medication errors that can occur.
CAUSES OF MEDICATION ERRORS
- Distraction : A nurse who is distracted may read “diazepam” as “diltiazem.” The outcome is not insignificant-if diazepam is accidentally administered, it could sedate the patient, or worse (e.g., if the patient has an allergy to the drug).
- Environment : A nurse who is chronically overworked can make medication errors out of exhaustion. Additionally, lack of proper lighting, heat/cold, and other environmental factors can cause distractions that lead to errors.
- Lack of knowledge/understanding : Nurses who lack complete knowledge about how a drug works, its various names (generic and brand), its side effects, its contraindications, etc. can make errors.
- Incomplete patient information : Lacking information about which medications a patient is allergic to, other medications the patient is taking, previous diagnoses, or current lab results can all lead to errors. Nurses who aren’t sure should always ask the physician or cross-check with another nurse.
- Memory lapses : A nurse may know that a patient is allergic, but forget. This is often caused by distractions. Forgetting to specify a maximum daily dose for an “as required” drug is another example of a memory-based error.
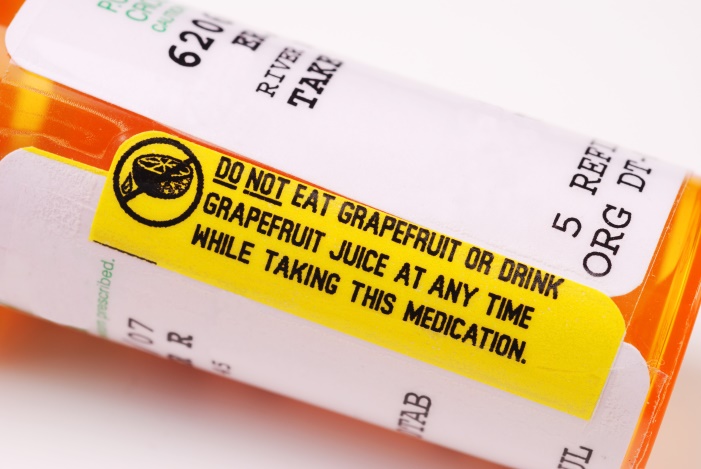
- Systemic problems : Medications that aren’t properly labeled, medications with similar names placed in close proximity to one another, lack of bar code scanning system, and other issues can lead to medical errors.

PREVENTING MEDICATION ERRORS
Nurses may not have the authority to make infrastructural changes, but they do have the power to suggest needed changes and take precautions to prevent medication errors, including the following:
KNOW THE PATIENT
This includes the patient’s name, age, date of birth, weight, vital signs, allergies, diagnosis, and current lab results. If patients have a barcode armband-use it. The added administration times of using arm band systems have led some nurses to create potentially dangerous “workarounds” to avoid scanning barcodes. Don’t make this potentially dangerous mistake- use all of the information at your disposal to ensure patient safety, and avoid shortcuts.
KNOW THE DRUG
Nurses need access to accurate, current, readily available drug information, whether the information comes from computerized drug information systems, order sets, text references, or patient profiles. If you have any questions or concerns about a drug, don’t ignore your instincts-ask. Remember that you are still culpable, even if the physician prescribed the wrong medication, the wrong dose, the wrong frequency, etc.
KEEP LINES OF COMMUNICATION OPEN
Breakdowns in communication among physicians, nurses, pharmacists, and others in the healthcare system can lead to medication errors. The “SBAR” method can help alleviate miscommunications. SBAR (Situation, Background, Assessment, Recommendation) works like this:
- Situation : “The situation is that Mr. Smith is complaining of chest pain.”
- Background : “He had hip surgery yesterday. About two hours ago he began complaining of chest discomfort. His pulse is 115, and he is short of breath and agitated.”
- Assessment : “My assessment is that Mr. Smith may be having a cardiac event.”
- Recommendation : “My recommendation is that you see him immediately, and that we start him on O2 and administer an analgesic immediately. Do you agree?”
Communication is vitally important, as it is the root cause of many sentinel events, according to the Joint Commission (TJC).5
DOUBLE CHECK HIGH ALERT MEDICINES
High-alert medicines such as heparin can have devastating consequences if not administered properly. A tragic case involving the death of three infant patients after receiving massive heparin overdoses happened as a result of misleading packaging. Since this incident, the drug manufacturer now uses larger font sizes, tear-off cautionary labels, and different colors to distinguish drug doses.6 Medications often look alike and sound alike-this can be a source of errors. Double check high alert medications with another nurse to prevent accidental overdoses and other medication errors.
DOCUMENT EACH DRUG ADMINISTERED
Accurate documentation is essential and should include accurate recording of the drug information, the name of the drug, the dose, route, time, patient response, and any refusal of the drug by the patient.
TAKE AN ACTIVE ROLE IN CORRECTING ISSUES YOU IDENTIFY
If you see that look-alike or sound-alike medications are stored next to each other, ask your supervisor to correct the problem, emphasizing the increased risk of medication errors. Request that medications be reconciled (i.e., that the names, dosages, and administration routes of all medications are compared to identify conflicts). Request that a bar coding system be implemented that allows for the verification of the six medication rights (right individual, right medication, right dose, right time, right route, right documentation).


INFORM THE PATIENT OF THE DRUGS THEY ARE RECEIVING
Make sure your patients know the names of the medications they are taking, what they look like, what they are for, how to take them or how they will be administered, the dosage, and the potential side effects and interactions.
ASK FOR CONTINUING EDUCATION
Ask for mandatory training sessions about medications that are introduced to your facility. Training should include medication-related policies, procedures, and protocols. Updates like these, along with comprehensive nurse CE programs that include healthcare videos, empower nurses and can help prevent medication errors.
Nurse educators and continuing education providers should include all of these prevention tips, and more, in nurse education programs to help nurses avoid medication errors that could have detrimental or even deadly consequences for patients, and significant consequences for nurses, including disciplinary action, job dismissal, criminal charges, and mental anguish.
Sources:
- http://iom.nationalacademies.org/~/media/Files/Report%20Files/1999/To-Err-is-Human/To%20Err%20is%20Human%201999%20%20report%20brief.pdf
- Medcom Trainex, “Medical Errors, Preventing Medication Errors” education video for healthcare professionals, 2015
- http://newsnetwork.mayoclinic.org/discussion/nearly-7-in-10-americans-take-prescription-drugs-mayo-clinic-olmsted-medical-center-find/
- http://www.fda.gov/Drugs/DrugSafety/MedicationErrors/ucm080629.htm
- http://www.jointcommission.org/assets/1/18/Root_Causes_Event_Type_2004-3Q_2015.pdf
- http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3462065/
